Alzheimer’s & Dementia Care At Home
Getting support with Alzheimer’s and dementia care at home helps loved ones to maintain dignity, wellbeing and independence. We’ve got years of experience to help you with whatever your family needs.
Why is dementia care so important?
Dementia is a condition that affects many people across the UK, but it’s not just the person living with dementia that feels the impact – families are affected too. At Home Instead, we understand the emotional and practical challenges families face when caring for a loved one with dementia. Our specialist care for dementia is designed to provide compassionate and expert care at home, where 82% of people believe that better care options would improve the lives of those affected, as reported in our recent New Ageing Index. We’re here to help families navigate this difficult journey, providing the highest level of care and support to ensure the best quality of life for your loved one.

Award winning dementia care training
At Home Instead, we take a pioneering approach to dementia care. Our unique programme, which is City & Guilds assured, is designed specifically for the home care environment. Developed with leading ageing experts, dementia specialists and key medical practitioners from around the world, it ensures your loved one receives the highest quality care tailored to their needs.
Our relationship-centred approach provides personalised care that:
- Helps your loved ones remain safe and calm at home
- Builds confidence and encourages engagement
- Provides nutritious meals and activities to encourage healthy eating
- Creates opportunities for social interaction
- Provides mind-stimulating activities
- Builds self-esteem and enhances physical strength
- Manages and soothes challenging behaviours
- Helps families take a rest from caring

How can we help?
We've helped thousands of families to stay safe, comfortable and happy at home. Whatever situation you're facing, or whatever the question is, Home Instead is here to help.
Are you in need of a little guidance right away?
03300 583450Other non-care-related enquiries
Home Instead have an experienced caring team that far exceeds in quality anything we experienced from other agencies at this point of service.
Steve, Client

I have had my care from Home Instead for almost ten years and things just keep getting better. I can’t praise them enough.
Kevan, Client
What we do to care for your loved ones
- We carefully match Care Professionals with clients to ensure a meaningful bond is created.
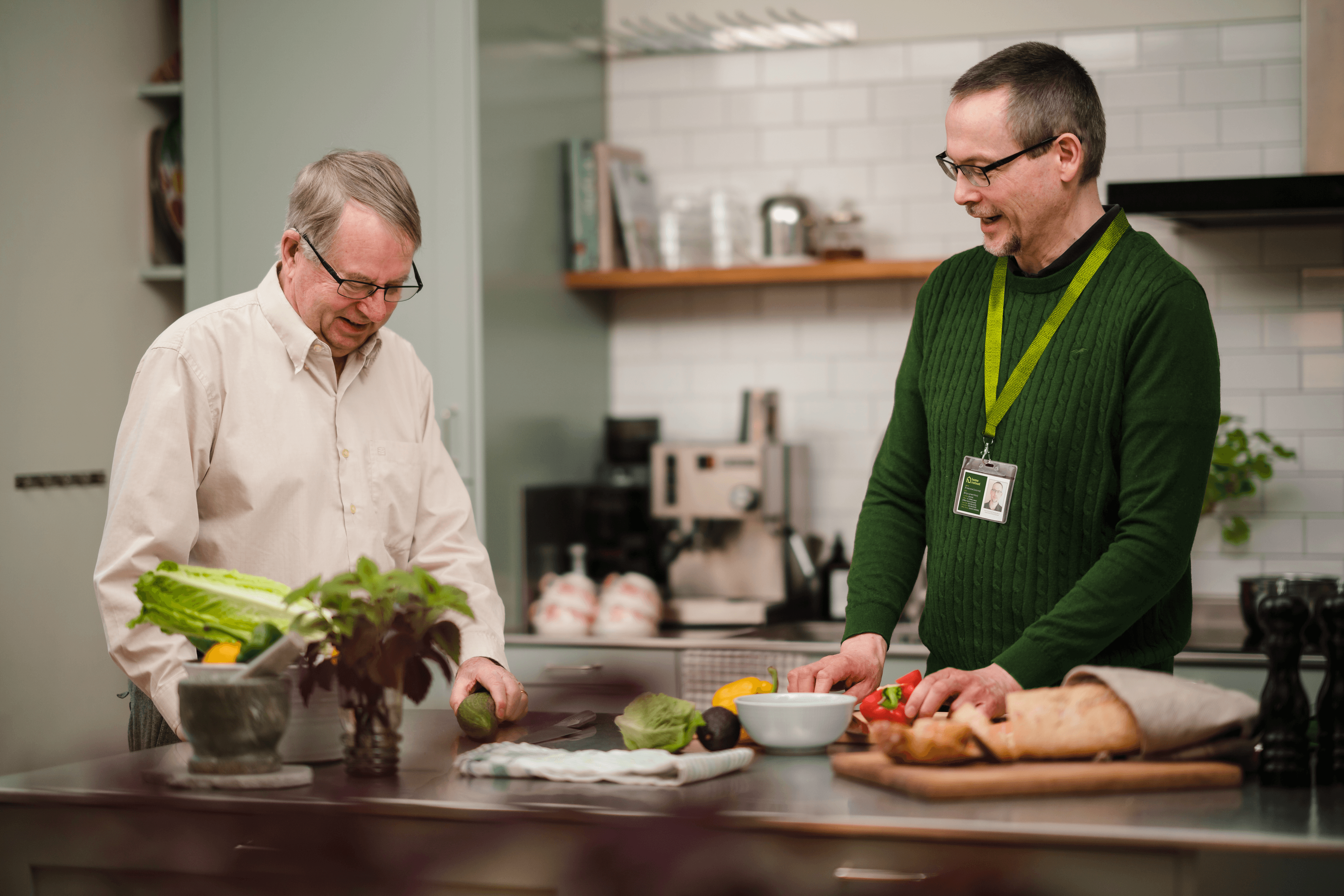
Home help & meal prep
Keeping the home environment clean, safe, and nourishing with home-cooked meals.Personal care
Assistance with bathing, dressing, and personal hygiene, always respecting the dignity of your loved one.Mobility support
Helping your loved one move around their home safely, including transfers and positioning.Health appointment management
We support your loved one to attend those important health appointments.Community engagement
We enable your loved one to continue to do the things you enjoy, be it a visit to the garden centre or your local art group.Transportation
Assistance getting your loved ones from A to B, whether it be to go visit a friend or help with their shopping.Medication management
Ensuring medicines are taken correctly and on time, supporting overall health.
Get in touch today to
see how we can help
Get in touch Guides

What Is dementia?
Discover more
What Is Alzheimer's?
Discover more
The different types of dementia
Discover more
Caring for someone with dementia at home
Discover more
What is dementia care?
Discover more
Building a care plan for a dementia patient at home
Discover more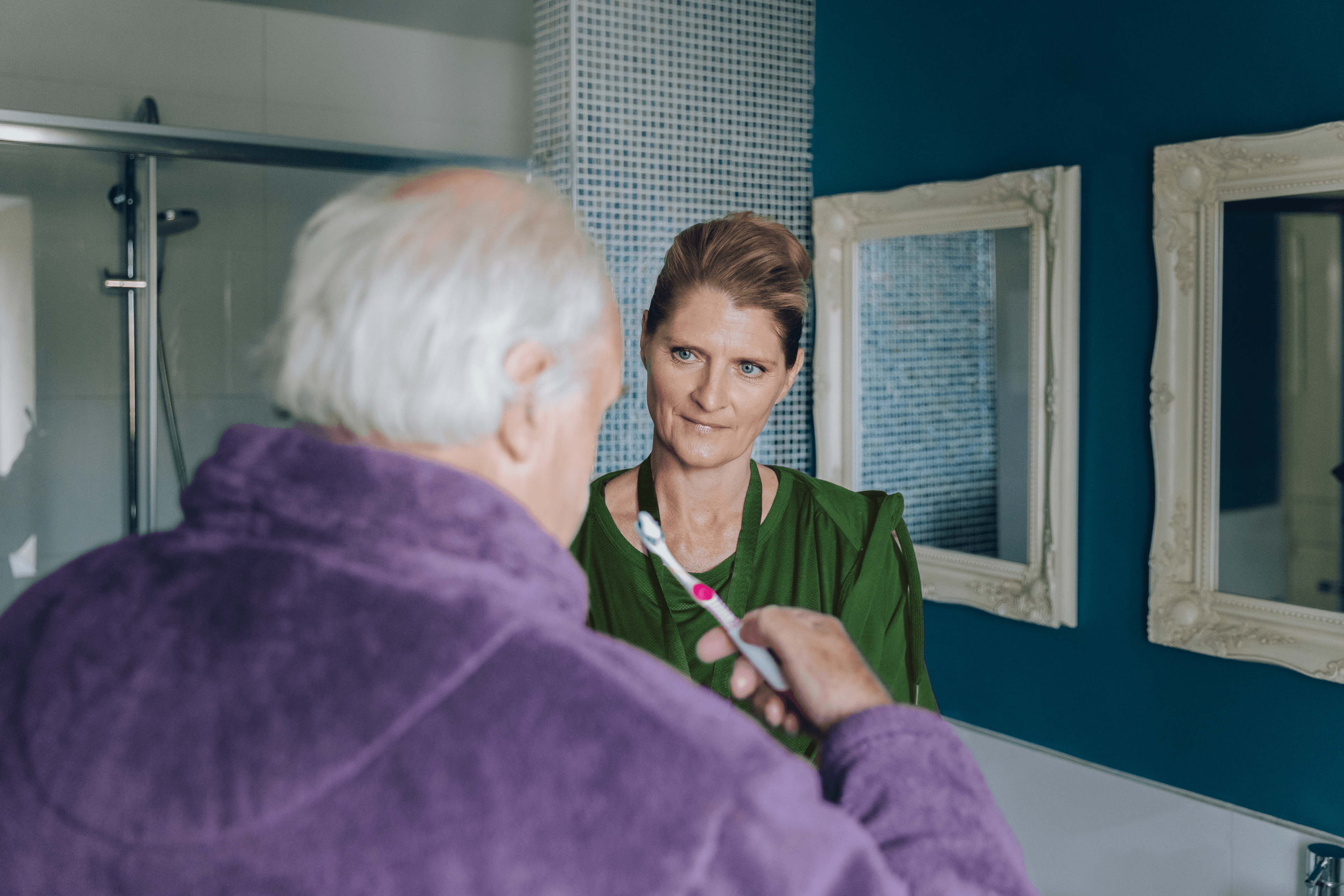
Overnight dementia care at home
Discover more
Making the care plan work: how to talk to someone with dementia
Discover more
Managing the stages of dementia
Discover more
What to know about rapid onset dementia
Discover more
What is "sundowning" in dementia?
Discover more
Understanding Dementia and Alzheimer's
Discover more
Considerations for Dementia Care
Discover more
Supporting Dementia at home
Discover more
What is a memory clinic?
Discover more
Dementia respite care
Discover more
How does dementia affect you emotionally?
Discover more
Vascular Dementia
Discover more
Understanding the 7 Stages of Lewy Body Dementia
Discover more
Understanding Posterior Cortical Atrophy (PCA) Dementia
Discover more
Understanding the 7 stages of frontotemporal dementia
Discover more
The physical symptoms off dementia
Discover more
Living with dementia: health & happiness
Discover more
Great games for dementia patients
Discover more
A guide to advanced dementia
Discover more
My spouse has dementia: what help can I get?
Discover more
What is the difference between Alzheimer's and dementia?
Discover more
Delirium vs dementia in older adults
Discover more
The benefits of dementia-friendly colours
Discover more
Home respite care for dementia patients
Discover more
Getting power of attorney for an ageing parent with dementia
Discover more
What to do if no power of attorney is set
Discover more
Doll therapy for dementia
Discover more
What to know about rapidly progressive dementia
Discover more
Mental Stimulation
Discover more
The cost of dementia care at home
Discover more
The best phones for people with dementia
Discover more
Home care for dementia and confabulation
Discover more
What does dementia feel like?
Discover more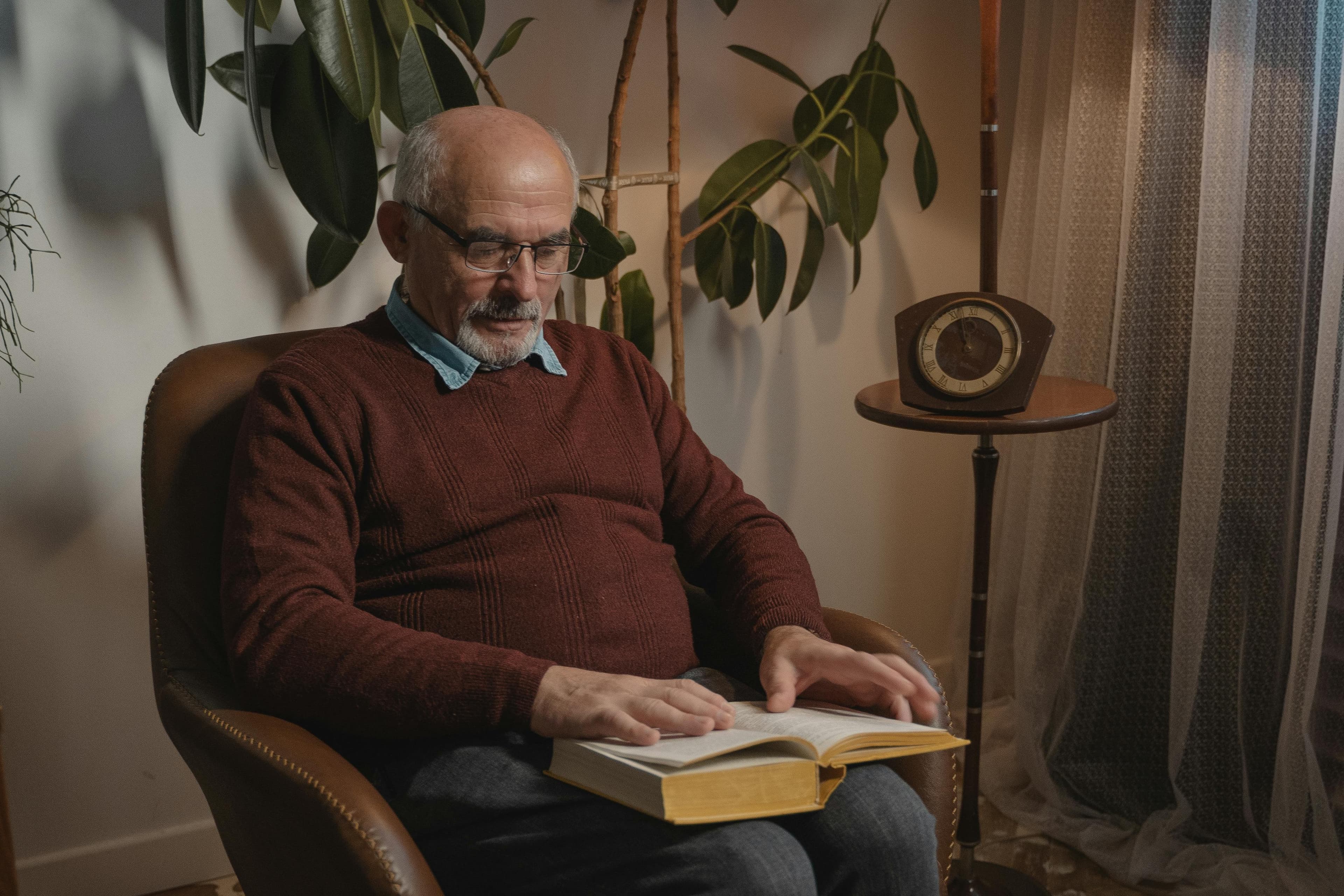
The best clocks for people with dementia
Discover moreperson centred care
Discover more
Elderly assistive devices
Discover moreWhat is a dementia village?
Discover more
Emergency dementia respite care
Discover more
OCD and dementia
Discover more
Dementia and seizures
Discover more
Does CBT for dementia work?
Discover more
Time shifting dementia
Discover more
Handling dementia and sexually inappropriate behaviour
Discover more
How dementia affects your social life
Discover more
Can alcohol cause dementia?
Discover more
Can you drive if you have a dementia diagnosis?
Discover more
Do statins cause dementia?
Discover more
Ideal gifts for people with dementia
Discover more
Fun questions to ask dementia patients
Discover more
Why is my loved one with dementia sleeping a lot?
Discover more
Dementia parents and staring
Discover more
What is dementia?
Dementia is a medical term for a collection of symptoms ranging from memory loss to impaired communication. It is caused by several conditions affecting neurons in the brain, and includes Alzheimer’s disease, Vascular dementia, dementia with Lewy Bodies, and many other types. If a person has dementia, their neurons are damaged which means electrical messages cannot be sent efficiently across them, which can impair some or all functions of the body.
The effects of dementia are often small to start with, but over time they can become severe enough to affect someone’s day-to-day life. The person’s symptoms will greatly depend on two primary factors; the parts of the brain affected, and the nature of the disease causing the dementia, but it can be extremely debilitating and distressing.

What is dementia care?
Dementia care is about understanding the condition and the many symptoms that can occur as each person living with dementia will have their own, unique experiences and challenges. Providing care to the whole person, not just the dementia symptoms, means understanding what that individual’s real world is and joining them in it, expressing empathy when needed and showing smiles while providing warmth and positive support.

Why choose dementia care at home?
As the saying goes, “Home is where the heart is”, and the best place for a person living with dementia is in their own home. This is where they will feel secure and comfortable, surrounded by their familiar possessions and loved ones.
Home Instead can provide flexible care to support you and your loved one, from a few hours a day or week for companionship and a bit of home help, all the way to full live-in care, including round the clock 24 hour care at home. Combined with knowledge and expert care from our dedicated Alzheimer’s and dementia Care Professionals, we can give you complete peace of mind.

Advice & Support

New Dementia Training
Discover more
Making communities dementia friendly
Discover more
Stepping into the shoes of someone with dementia with Training2Care’s Dementia Bus
Discover more
Supporting refugees with Family Dementia guide
Discover more
What’s the difference between dementia and Alzheimer's?
Discover more
A guide to dementia care
Discover more
FAQ's
- What are the benefits of dementia care at home?
With the right care and support, a person living with dementia can be as independent as possible. Dementia home care can enable them to live happily and securely in their own home, in familiar surroundings, surrounded by people they know.
- I have dementia / my loved one has dementia. Can you help me?
Yes. We understand how difficult it can be caring for someone living with dementia but we have years of experience in helping families cope with the situation at home. Our City & Guilds Assured dementia training programme ensures that our Care Professionals are fully equipped to provide exceptional care for individuals living with all types of dementia.
- What is the most common type of of dementia in the UK?
Alzheimer’s disease is the most common type of dementia, followed by Vascular dementia and then dementia with Lewy Bodies.
Discover More - What are some of the possible symptoms of dementia?
- Difficulties with problem solving
- Memory impairment
- Memory lapses
- Struggle to find words
- Difficulty processing information
- Difficulty making sense of what is seen
- Recognising people and places
- Changes in mood and behaviour
- Will my loved one have to give up their pet now they have been diagnosed with dementia?
When someone is diagnosed with dementia, it is often assumed that keeping their beloved pet is impossible. This is not necessarily the case. Studies have shown that pets have actually been known to increase the health of those with dementia while providing them with a friend to spend their time with. Owning a cute and cuddly companion can even be an essential part of their daily routine. Before jumping to any conclusions, it may be beneficial to review all of your options when it comes to this important decision.
An unexpected diagnosis can be frightening or difficult, and some might discover that they want their pet to remain by their side. After considering the following factors, you may find that there are other alternatives to immediately giving up a best friend.
Discover More - How can I help my loved one when they have dementia?
For people living with dementia and Alzheimer’s, lack of stimulation and boredom can be one of the most frustrating things. It’s important to provide activities that engage and bring pleasure to people living with Alzheimer’s and dementia.
Stimulating activities can help keep them in high spirits and prevent them from developing depression, whilst lessening anxiety and irritability.
Activities should aim to:
- Stir memories and allow them to reminisce about their life
- Foster emotional connections with others – contact with others is vital
- Encourage self-expression
- Make them feel more engaged with life
- Help them feel productive
- My loved one with Dementia has begun to develop aggressive behaviour, can you give me any advice?
If you have a relative with dementia – perhaps you are their carer – you may be aware that at some point you might find yourself dealing with aggressive behaviour from them. This is a prospect that many people fear, but there are ways to cope with such challenging behaviours.
Discover More - Are there warning signs that I or my loved one are getting dementia?
The early stages of dementia are not always obvious, and symptoms and problems might develop slowly. To add to these difficulties, early signs of Alzheimer’s and dementia are frequently easy to dismiss as a normal sign of ageing. However, if you know what to look out for, you can keep an eye on yourself and your loved ones and identify symptoms early. This will allow you to get the medical advice early on and work out care ahead of time.
Discover More - This is my loved ones first Christmas after being diagnosed with dementia, is there any advice you can give?
For a person with dementia, Christmas poses challenges that include disruption to a routine, confusing changes to décor and the layout of a home, and the pressure to be social over extended periods of time. When somebody’s memory or cognitive skills are deteriorating, they will find these tasks especially difficult; it is important that they are catered for in the most sensitive ways possible.
By looking at each potential challenge in turn, we have suggested some ways to manage these difficulties and have a successful Christmas without causing your loved one with dementia distress or exacerbating their confusion.
Discover More - What is the difference between dementia and Alzheimer’s disease?
There are many types of dementia. Alzheimer’s disease is simply one form of dementia.
Learn More - Where did the name ‘Alzheimer’s’ come from?
Dr. Alois Alzheimer is credited with discovering Alzheimer’s disease. Dr. Alzheimer was a well-known and popular German physician and researcher working in the early 1900s. Physicians and scientists at the time had a fascination with the human brain and were studying it to better understand how it worked.
Dr. Alzheimer met Auguste Deter, the first person who was diagnosed with Alzheimer’s. Auguste told Dr. Alzheimer, “I have forgotten myself”. He brought her to the doctor when she started to have memory loss and delusions. Dr. Alzheimer studied her for several years, noting her decline.
Because of Dr. Alzheimer’s discovery, the disease was named after him.
- I have Alzheimer’s disease/my loved one has Alzheimer’s disease. Can you help me?
Certainly. We know how challenging it can be caring for someone living with Alzheimer’s disease, however we have years of experience in helping families cope with the situation at home. Our City & Guilds Assured dementia training programme means our Care Professionals are trained to care for people living with all the different types of dementia.